
Introduction: What is Chronic Venous Insufficiency (CVI)?
Chronic Venous Insufficiency ICD‑10 : A Human‑Centered Guide to Understanding, Coding & Care Chronic venous insufficiency (CVI) is a condition in which the veins in the legs cannot properly return blood to the heart. There are two types of veins in our blood vessels: deep veins and superficial veins. These veins have small valves that push blood in a one-way flow toward the heart and prevent it from flowing backward against gravity.
When these valves are damaged or weakened, blood begins to pool in the veins of the legs, which puts pressure on the veins. Over time, this increased pressure causes the veins to dilate and weaken the walls of the blood vessels, preventing blood from flowing properly. This condition is called chronic venous insufficiency.
The Place of CVI in ICD-10
There is an internationally recognized system for diagnosing and classifying diseases in medicine, called the International Classification of Diseases (ICD). It is published by the World Health Organization (WHO) and is currently in its tenth edition (ICD-10).
ICD-10 contains specific codes for CVI, which medical professionals use to diagnose, collect data, and perform statistical analysis. Different ICD-10 codes are used for different forms of CVI, depending on the severity of the disease and associated complications. For example:
- I87.2: Chronic venous insufficiency (peripheral) – This is usually used for common CVI.
- I83.9: Varicose veins without inflammation or ulceration – when varicose veins are present but there is no inflammation or ulcer.
- I83.0: Varicose veins of lower extremities with ulcer – when varicose veins are accompanied by ulcer.
- I83.2: Varicose veins of lower extremities with both ulcer and inflammation – when varicose veins are accompanied by ulcer and inflammation.
These codes are very important for doctors because they help in making an accurate diagnosis, facilitate the development of a treatment plan, and create a common language for communication within the health system.
Why does CVI occur? Causes and risk factors
The causes of CVI are multiple and often multiple factors work together. Some common causes and risk factors are mentioned below:
- Genetic predisposition: If someone in your family has CVI, you are more likely to develop CVI. This is an important risk factor.
- Age: As you age, veins and valves become weaker, increasing your risk of developing CVI. It is usually more common in people over 50 years of age.
- Gender: Women are more prone to CVI, especially during pregnancy and hormonal changes. During pregnancy, the growing uterus puts pressure on the veins, and hormonal changes relax the veins.
- Obesity: Excess weight puts extra pressure on the veins in the legs, which can damage the valves.
- Standing or sitting for long periods of time: People in professions that require standing or sitting for long periods of time (e.g. teachers, surgeons, office workers) are at higher risk of developing CVI. Staying in the same position for long periods of time slows down blood circulation in the legs.
- Physical inactivity: Lack of regular exercise weakens the leg muscles. The leg muscles act like a pump and help push blood towards the heart. When the muscles are weak, blood circulation becomes difficult.
- Blood clots (Deep Vein Thrombosis – DVT): The risk of developing CVI is greatly increased if you have a history of blood clots in the legs in the past. DVT damages the inner lining of the veins and makes the valves ineffective. This is called post-thrombotic syndrome.
- High blood pressure: Although not a direct cause, high blood pressure can put extra pressure on the veins.
- Smoking: Smoking damages blood vessels and impairs blood circulation.
- **Injury**: Any serious injury or surgery to the legs can damage the veins.
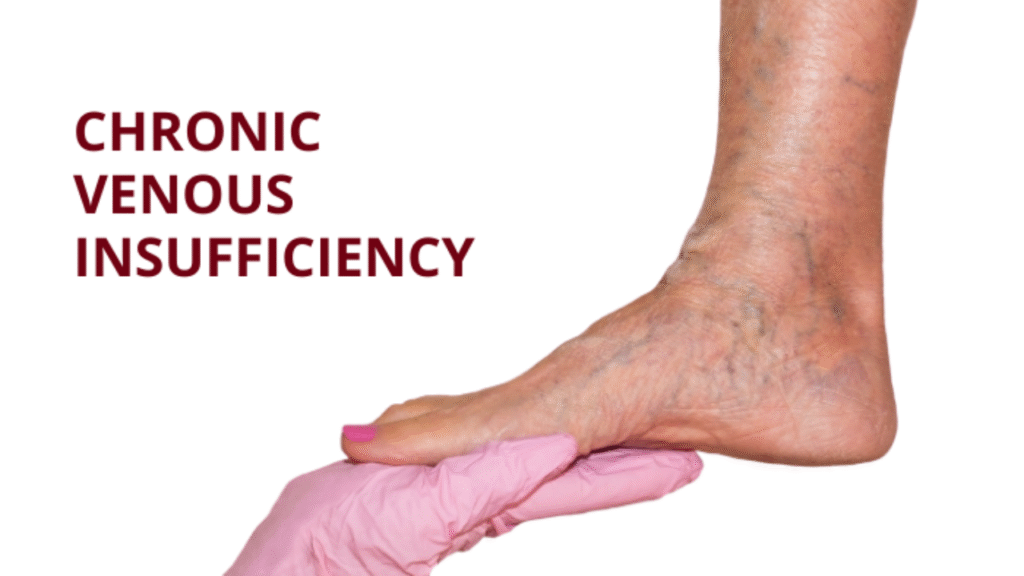
Symptoms of CVI
The symptoms of CVI can vary in severity and get worse over time. In the early stages, the symptoms may be mild and many people confuse it with simple fatigue or pain. However, over time, the symptoms become more obvious and severe.
Early symptoms:
- Pain, heaviness, or fatigue in the legs: This feeling is especially intense at the end of the day or after standing for a long time.
- Swelling in the legs: Swelling in the ankles or lower legs, which increases at the end of the day and decreases at night when the legs are elevated.
- Itching in the legs: The skin may feel itchy, especially on the ankles and below the knees.
- Leg cramps or spasms: The muscles in the legs may tense or spasm at night.
- Varicose veins: The veins on the back of the legs become swollen, twisted, and appear bluish.
Advanced symptoms:
Skin discoloration (Stasis Dermatitis): The skin on the legs may become brown or reddish due to prolonged blood pooling. This is most common on the ankles and below the knees.
- Thickening and hardening of the skin (Lipodermatosclerosis): The tissues under the skin harden, making the skin look thick and tight.
- Eczema: Dryness, redness, and rash may occur on the skin.
- Leg ulcers or sores (Venous Ulcers): This is the most serious complication of CVI. Usually, small injuries around the ankles can easily turn into sores that do not heal. These sores can be very painful and are at risk of becoming infected.
- Infection (Cellulitis): Swelling, redness, and severe pain in the skin of the legs may indicate a bacterial infection.
If you have any of these symptoms, it is very important to seek medical attention immediately.
How is CVI diagnosed?
To diagnose CVI, a doctor will first take a complete health history and perform a physical exam. The following procedures help diagnose CVI:
- Physical exam: The doctor will examine the patient’s legs, checking for swelling, changes in skin color, varicose veins, and any ulcers. He or she will ask about the patient’s symptoms in detail.
- Duplex Ultrasound: This is the most important test for diagnosing CVI. This procedure uses sound waves to see the flow of blood through the veins and check the function of the valves. It also provides information about the presence of any blockages or blood clots inside the veins.
- Volume Plethysmography: This test measures blood flow in the legs and evaluates the function of the valves in the veins.
- Venography: This is a special X-ray test, in which a contrast dye is injected into the veins, which makes the veins visible on the X-ray image. It helps identify problems inside the veins. However, it is usually done when DVT is suspected or when other tests are inconclusive.
- MRI Venography or CT Venography: In some cases, these tests may be done to get a more detailed picture, especially when deep vein thrombosis is suspected.
Treatment of CVI
The treatment of CVI depends on the severity of the disease and symptoms. The main goals of treatment are to relieve symptoms, prevent complications, and improve quality of life. Treatment methods are generally divided into two categories: conservative management and invasive procedures.
Conservative Management:
1. Lifestyle changes:
- Regular exercise: Exercise such as walking, swimming, or cycling strengthens the leg muscles and helps with blood circulation. It is especially important to keep the leg muscles active.
- Weight control: Obesity is a major risk factor for CVI, so keeping your weight under control is very important.
- Avoid prolonged standing or sitting: If your job requires you to stand or sit for long periods of time, take regular breaks to walk or move your legs.
- Elevate your legs: Keep your legs higher than your heart while sleeping or resting. This helps blood return to the heart and reduces swelling.
- Wear loose clothing: Avoid wearing tight clothing, especially around the waist, as it can restrict blood flow.
2. Compression Therapy:
- Compression Stockings: This is the most important and effective treatment for CVI. Compression stockings create even pressure on the legs, which constricts the veins and helps push blood back to the heart. They also help reduce swelling. Socks are available in different pressures and lengths, and the right one should be selected as per the doctor’s advice.
3. Skin care:
- Regular moisturizing: The skin of people with CVI becomes dry and brittle, so it is important to use moisturizer regularly.
- Ulcer prevention and treatment: If ulcers develop, regular cleaning and dressing are essential. Antibiotics may be needed if there is a risk of infection.
4. Medication:
- Diuretics: Diuretics may be used in some cases to reduce swelling, but they do not treat the underlying cause of CVI.
- Flavonoids: Some natural ingredients, such as diosmin and hesperidin, help strengthen vein walls and reduce inflammation.
- Antibiotics: If there is a skin infection (cellulitis), antibiotics are needed.
- Anti-inflammatory drugs: Non-steroidal anti-inflammatory drugs (NSAIDs) can be used to reduce pain and inflammation.
Invasive Procedures:
When conservative treatments fail to control symptoms or the disease progresses to a severe stage, the following procedures may be considered:
- Sclerotherapy: In this procedure, a special chemical substance (sclerosant) is injected directly into small or medium-sized varicose veins. This chemical irritates the inner wall of the vein, causing the vein to close and eventually disappear. It is effective for small and medium varicose veins.
- Laser Ablation or Radiofrequency Ablation (RFA): This is a popular and minimally invasive procedure for CVI. In this procedure, a catheter is inserted into the vein and the inner wall of the vein is heated using laser or radiofrequency energy. This heat shrinks and closes the vein. The blocked vein is absorbed by the body over time and blood flows through other healthy veins. This procedure is effective for large varicose veins.
- Ambulatory Phlebectomy: In this procedure, varicose veins are removed from under the skin through small incisions. It is done under local anesthesia and does not take much time.
- Venous Stripping: This is a traditional surgical procedure, which is rarely used today because less invasive methods such as laser or radiofrequency ablation are available. In this procedure, a large damaged vein is completely pulled out using a long wire. It is usually considered for large and severe varicose veins.
- Venous Ulcer Dressing and Management: If ulcers develop, it is very important to ensure proper dressing, infection control, and adequate nutrition. In some cases, special dressings and vacuum-assisted closure (VAC) therapy may be used.
Complications of CVI:
If CVI is left untreated, it can lead to several serious complications:
- Skin ulcers (Venous Ulcers): This is the most common and painful complication. These ulcers can be difficult to treat and may recur.
- Infection (Cellulitis): Bacteria can enter through skin ulcers or cracks, causing infection.
- Bleeding: Varicose veins can rupture and bleed.
- Superficial Thrombophlebitis: Inflammation and blood clots in the superficial veins.
- Deep Vein Thrombosis (DVT): Although not a direct complication of CVI, people with CVI are at slightly higher risk of developing DVT. DVT is a serious condition that can cause a blood clot in the lungs (Pulmonary Embolism), which can be fatal.

What to do to prevent CVI
Although it is not possible to change the genetic predisposition to CVI, there are steps you can take to reduce your risk and slow its progression:
- Regular exercise: This helps blood flow and keeps veins healthy.
- Maintaining a healthy weight: Excess weight reduces pressure on veins.
- Avoiding prolonged standing or sitting: Take breaks between work and move your legs.
- Elevating your legs: Keep your legs slightly elevated at the end of the day or while sleeping.
- Avoiding tight clothing: Wear loose clothing.
- Quitting smoking: Smoking damages blood vessels.
- Doctor’s advice: If you experience symptoms of CVI, seek medical advice quickly. Starting treatment at an early stage can prevent complications.
Frequently asked questions (FAQs) about Chronic Venous Insufficiency ICD‑10
1. Is CVI curable?
Although CVI is not completely curable, its symptoms can be controlled and complications can be prevented with proper treatment and lifestyle changes. Some invasive procedures remove damaged veins, but there is a risk of CVI developing in new veins.
2. Is CVI life-threatening?
CVI is usually not life-threatening. However, its complications, such as deep vein thrombosis (DVT) and pulmonary embolism, can be life-threatening. Also, ulcers caused by CVI can become infected and become serious if left untreated.
3. Is CVI normal during pregnancy?
Yes, CVI and varicose veins are common in women during pregnancy. During pregnancy, the growing uterus puts pressure on the pelvic veins and hormones like progesterone relax the blood vessel walls. Symptoms usually improve after delivery, but in some cases they can be long-lasting.
4. When should compression stockings be worn?
Compression stockings should usually be worn first thing in the morning after waking up and removed at night before going to bed. This helps to reduce swelling and discomfort during the day. It is important to choose the right size and pressure as recommended by your doctor.
5. Does diet play a role in preventing CVI?
There is no specific diet that can directly prevent CVI, but a balanced and healthy diet can help control weight, which can help reduce the risk of CVI. Foods rich in fiber prevent constipation, which can help reduce pressure on the veins. Drinking enough water is also important.
6. Is CVI the same as varicose veins?
CVI and varicose veins are related, but not the same. Varicose veins are enlarged, twisted veins that appear under the skin, and can be a symptom or consequence of CVI. CVI is a blood circulation problem caused by the malfunctioning of the valves in the veins, which can cause other symptoms in addition to varicose veins.
7. When should you see a doctor for CVI?
If you experience swelling, pain, heaviness, skin discoloration, itching, ulcers, or varicose veins in your legs, you should seek medical attention immediately. Early treatment can prevent the progression of the disease and avoid complications.
Conclusion
Chronic venous insufficiency (CVI) is a common health problem that affects millions of people around the world. Its symptoms are often confused with common fatigue or pain, which can lead to many people not seeking treatment at the right time. In this article, we have discussed the causes, symptoms, diagnosis and treatment of CVI in detail, through which we hope you have got a clear idea about CVI. Remember, lifestyle changes are very important in preventing CVI and it is essential to seek medical advice quickly if you experience its symptoms. With timely and proper treatment and care, it is possible to avoid the complications of CVI and live a better life. Your health is in your hands!

Hi, I’m M Saif, a digital marketer with a strong focus on SEO and content writing. I help businesses improve their online visibility, drive organic traffic, and create engaging content that converts. With a results-driven approach, I work on strategies that not only boost rankings but also deliver real value to audiences.







Leave a Reply